Bipolar disorder causes intense shifts between euphoric highs and devastating lows. This mental health condition occurs because of complex biological events rooted in the brain’s intricate chemistry. Understanding the science behind mood swings in bipolar disorder can demystify the experience, providing clarity and a sense of control.
For individuals and their loved ones, these mood episodes can be confusing and distressing. You may wonder what causes these dramatic changes and why they feel so powerful. The answer lies deep within the brain’s structure and function.
This post will guide you through the key scientific discoveries that help explain the intense mood episodes of bipolar disorder. We will look at the role of neurotransmitters, brain structure, genetics, and environmental factors. Our goal is to offer a compassionate, reassuring, and professional overview that helps you feel seen, heard, and supported on your path to wellness.
The Brain’s Chemical Messengers: Neurotransmitters
At the core of brain function are neurotransmitters, the chemical messengers that allow nerve cells (neurons) to communicate. In bipolar disorder, it’s believed that an imbalance in several key neurotransmitters influences mood regulation. Think of these chemicals as a complex orchestra; when one section is out of tune, it affects the entire symphony.
Dopamine
Three primary neurotransmitters are consistently implicated in bipolar disorder: dopamine, serotonin, and norepinephrine. There’s a link between dopamine and the brain’s reward and pleasure centers.
During manic episodes, dopamine activity skyrockets, contributing to feelings of euphoria, increased energy, and risky behaviors. Conversely, a dip in dopamine function can contribute to the lack of pleasure and motivation experienced during depressive episodes.
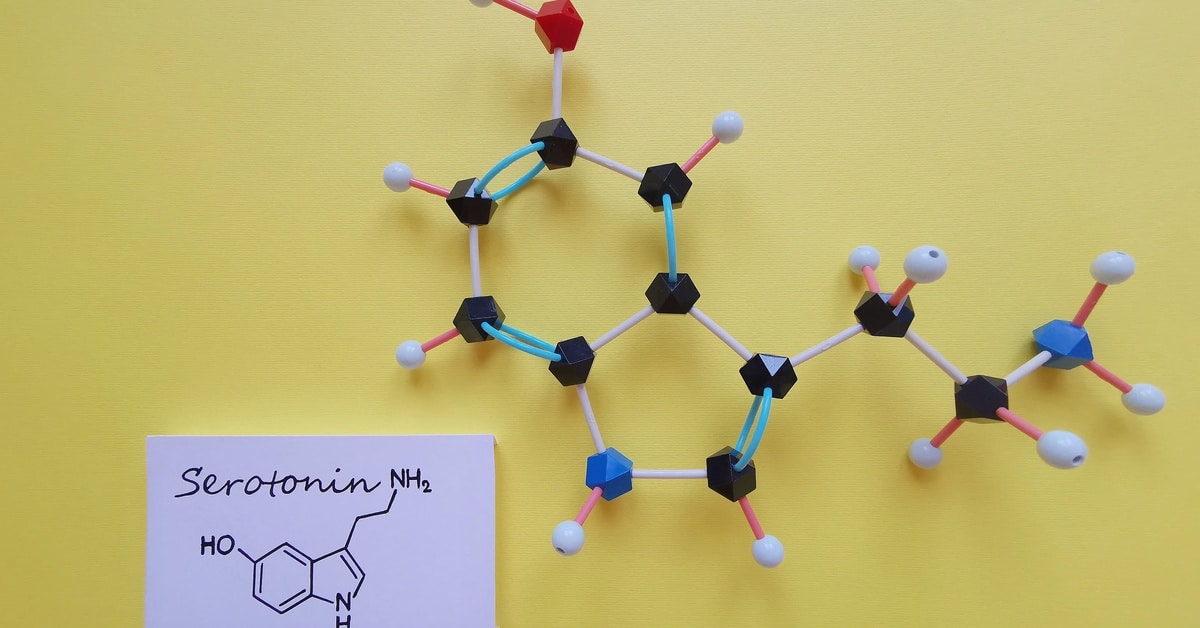
Serotonin
Serotonin regulates people’s mood, sleep, and appetite. While low serotonin levels have long been associated with depression, its function in bipolar disorder is more complex. The interplay between serotonin and other neurotransmitters likely contributes to the cycling between mania and depression.
Norepinephrine
Bipolar disorder can also occur due to dysregulated norepinephrine. It’s involved in the body’s fight or flight response. Elevated levels cause high energy and restlessness, which scientists associate with mania. There’s also a connection between decreased levels and the fatigue and sluggishness of depression.
Brain Structure and Circuitry in Bipolar Disorder
Beyond brain chemistry, researchers can use neuroimaging to observe structural and functional differences in the brains of people with bipolar disorder. These are not signs of damage but rather variations in how certain brain regions develop and how they communicate with one another. These differences help explain the challenges with emotional regulation and impulse control that characterize the condition.
The prefrontal cortex, located at the front of the brain, is the command center for decision-making, problem-solving, and managing emotions. In individuals with bipolar disorder, this area commonly shows reduced activity. This can make it difficult to rein in the intense emotions generated by deep brain structures, such as the amygdala.
The amygdala acts as the brain’s emotional alarm system. It processes fear, excitement, and many other strong feelings. In bipolar disorder, the amygdala is typically overactive, sending out powerful emotional signals. A prefrontal cortex that is unable to effectively moderate these signals causes extreme highs of mania or the profound lows of depression. This disconnect between the brain’s thinking and feeling centers is a key feature of the disorder’s neurobiology.
Other brain regions, like the hippocampus (involved in memory and learning) and the basal ganglia (involved in motor control and reward), also show differences. This complex network of interconnected brain circuits helps explain why bipolar disorder affects people’s mood, energy, sleep, thinking, and behavior. Understanding this helps frame the condition as a whole-brain disorder, not just an emotional one.
The Genetic Connection
Bipolar disorder has a strong genetic component, meaning it often runs in families. While having a relative with the condition does not guarantee you will develop it, it does greatly increase your risk. There are several genes that may contribute to the likelihood of developing bipolar disorder. The genes are not a bipolar gene but rather a collection of genetic variations that influence brain development and neurotransmitter systems.
For example, some genes create proteins that transport neurotransmitters or build receptors for them on neurons. A slight variation in one of these genes could make the brain’s chemical signaling system more vulnerable to an imbalance. Other identified genes relate to the body’s internal clock or circadian rhythms, which could explain why disrupted sleep is a common trigger and symptom of mood episodes.
It is important to remember that genetics is only part of the story. Many people with these genetic risk factors never develop bipolar disorder. This is where environmental factors come into play, acting as potential triggers that interact with an individual’s genetic vulnerability.
Environmental Triggers and Life Stress
Genetics might set the foundation for bipolar disorder, but environmental factors cause the mental health condition to affect the individual’s behavior. Substantial stress is one of the most common triggers for the onset of bipolar disorder and for subsequent mood episodes in those who are already diagnosed. Events such as trauma, major life changes, and the loss of a loved one can disrupt the delicate balance of the brain’s chemistry.
Sleep deprivation is another powerful trigger. The body’s circadian rhythm is closely related to mood regulation. Disruptions to a consistent sleep-wake cycle can destabilize brain activity and precipitate a manic or depressive episode.
Substance use can also have a profound impact on one’s mental health. Alcohol and drugs directly alter brain chemistry, thereby interfering with the effectiveness of medications and triggering mood episodes. Even seemingly harmless substances, like caffeine, can disrupt sleep and increase anxiety. Recognizing and managing various environmental factors and personal habits are important to establishing a comprehensive treatment plan.

How Treatment Works With the Brain
Mood Stabilizers
Mood stabilizers, the primary class of medication used, work by targeting the underlying neurobiological issues. For instance, lithium, one of the most effective treatments, can strengthen connections between neurons and regulate neurotransmitter activity, creating a more stable internal environment.
Antipsychotic Medications
Antipsychotic medications can help manage the symptoms of mania by moderating dopamine levels. Psychiatrists cautiously administer antidepressants to lift depressive episodes, often in combination with a mood stabilizer to prevent a switch into mania. Finding the right medication or combination of medications is a collaborative process between you and your psychiatrist because no two people have the same brain chemistry and symptoms.
Psychotherapy
Psychotherapy, such as cognitive-behavioral therapy (CBT), helps individuals develop skills to manage the condition. Therapy teaches people how to recognize the early warning signs of a mood shift, develop coping strategies for stress, and maintain healthy routines. A combination of medication and therapy provides a powerful, two-pronged approach to managing bipolar disorder by addressing both the biological and behavioral aspects of the condition.
By learning the science behind mood swings in bipolar disorder, you can move from a place of confusion to one of understanding and empowerment. This knowledge reinforces that bipolar disorder is a medical condition, not a personal failing, and that effective, evidence-based treatments are available.
The healthcare professionals at Envision Mindcare are ready to help you improve your mental health and quality of life. Every patient receives a personalized bipolar disorder treatment plan. Book a consultation to start the journey toward wellness through our multifaceted approach.

